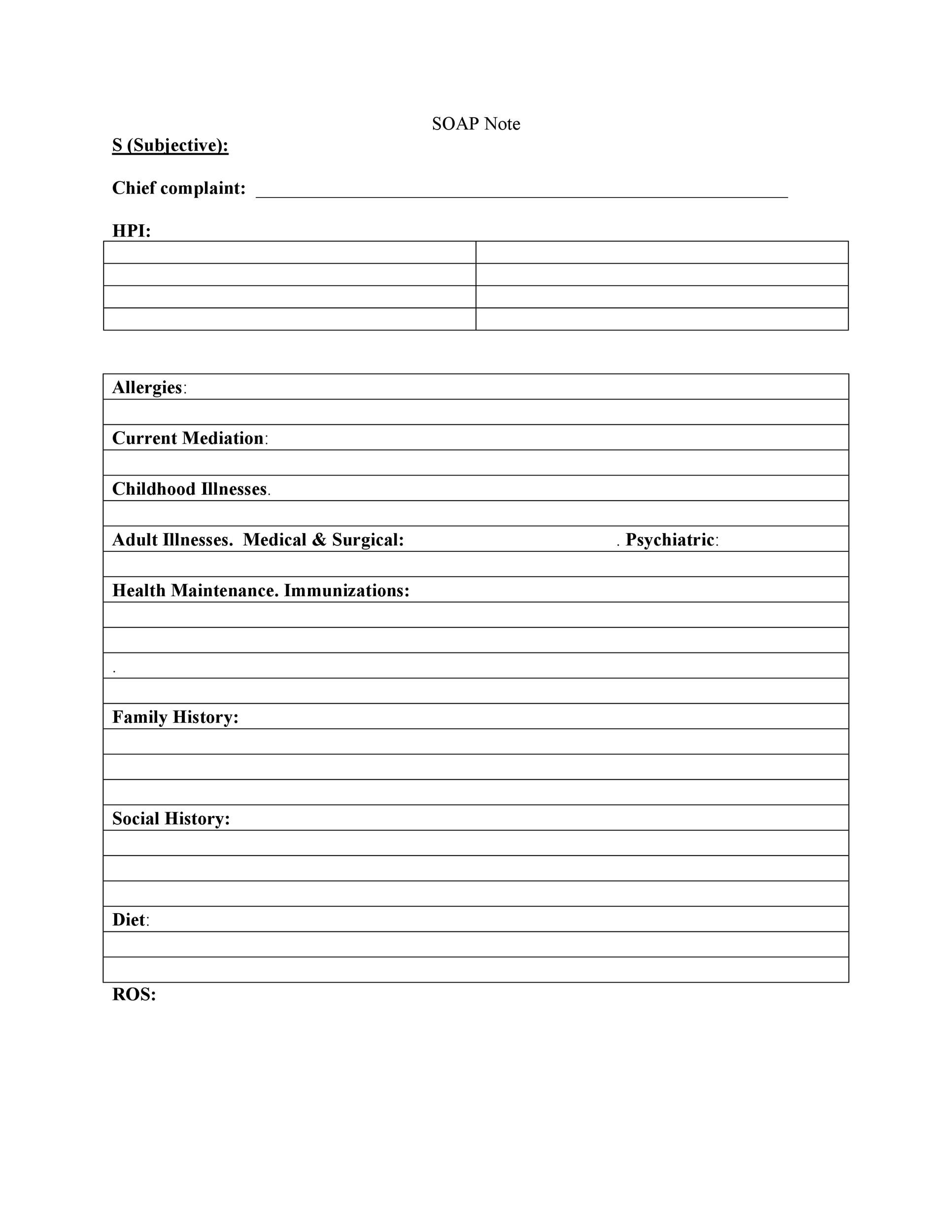
**Why Soap Notes Are Reshaping Healthcare Documentation in the US** In today’s fast-evolving digital world, healthcare professionals are increasingly turning to structured documentation tools—not just for compliance, but as a strategic way to streamline workflows and enhance communication. One such tool gaining quiet momentum is the soap notes format. Though rooted in clinical practice, its growing relevance reflects broader shifts toward clarity, efficiency, and transparency in patient care. This article explores how soap notes are becoming a trusted method for recording medical assessments, why guidance around them matters now more than ever, and what users truly need to understand—without jargon, risk, or compromise. **Why Soap Notes Is Gaining Attention Across the US** The rise of soap notes parallels a deeper demand for precision and consistency in healthcare documentation. In a mobile-first environment where time and accuracy are critical, professionals seek a clear, standardized template that integrates seamlessly with digital platforms. Beyond efficiency, the cultural push for better patient-provider communication has spotlighted the role of concise, well-organized communication—soap notes deliver just that. Additionally, increasing awareness around data interoperability and EHR optimization positions soap notes as a foundational practice for future-ready clinics. While still not mainstream in public conversation, interest is growing quietly—driven by real, practical benefits. **How Soap Notes Actually Works**
**Common Questions People Have About Soap Notes** **What makes soap notes different from regular clinical notes?** Soap notes provide a standardized, modular structure that enhances clarity and consistency—something free-text notes often lack. This structure supports better data extraction, improves legibility, and reduces errors in high-pressure environments. **Are soap notes required in all US healthcare settings?** They are not mandated by regulation, but their use is growing by choice. Clinics seeking efficiency, compliance, or improved care coordination increasingly adopt soap notes as a best practice. **How long should a soap note entry be?** Best practice favors brevity and focus—aim for 2–3 concise sentences per component. This ensures readability, especially on mobile devices, where thick text harms engagement and understanding. **How do soap notes support digital health goals?** Their clear, consistent format integrates smoothly with electronic health records (EHRs) and health data systems. This alignment helps with interoperability, analytics, and long-term data integrity across platforms. **Opportunities and Considerations** Soap notes offer clear advantages: improved documentation accuracy, faster provider coordination, and stronger patient data visibility. They also align with broader industry trends toward transparency and digital readiness. However, success depends on consistent application and staff training—rushing entries or ignoring structure undermines value. Additionally, while soap notes improve clarity, they are not a substitute for professional medical judgment; their role is supportive, not determinative. **Things People Often Misunderstand About Soap Notes** Contrary to misconceptions, soap notes are not a rigid checklist nor an administrative burden. They are a communication tool designed to reflect clinical reasoning in a way that’s accessible, traceable, and reliable. Many also believe they require specialized software, but simple word processors or EHRs can support the format effectively. The key is consistent, intentional use—not perfection on the first draft. **Who Soap Notes May Be Relevant For** While most commonly used by clinicians to structure patient records, soap notes serve diverse users in the healthcare ecosystem. Administrators rely on them for workflow analysis and compliance reporting. Medical students find the format a helpful scaffold for learning clinical reasoning. Even patients benefit indirectly—far clearer documentation supports better informed consent and care continuity. The neutral, patient-centered nature makes soap notes adaptable across roles and settings. **Soft CTA: Keep Evolving with the Future of Care** Soap notes are more than a trend—they’re a practical step toward smarter, more transparent healthcare. By grounding documentation in clarity and consistency, they empower professionals, strengthen patient trust, and prepare organizations for digital progress. Whether you’re a clinician seeking efficiency, a leader evaluating workflow tools, or someone curious about modern care practices, exploring soap notes offers valuable insight. In a landscape where careful, accurate communication shapes outcomes, soap notes are quietly leading the way—without losing sight of what matters most: people.
While most commonly used by clinicians to structure patient records, soap notes serve diverse users in the healthcare ecosystem. Administrators rely on them for workflow analysis and compliance reporting. Medical students find the format a helpful scaffold for learning clinical reasoning. Even patients benefit indirectly—far clearer documentation supports better informed consent and care continuity. The neutral, patient-centered nature makes soap notes adaptable across roles and settings. **Soft CTA: Keep Evolving with the Future of Care** Soap notes are more than a trend—they’re a practical step toward smarter, more transparent healthcare. By grounding documentation in clarity and consistency, they empower professionals, strengthen patient trust, and prepare organizations for digital progress. Whether you’re a clinician seeking efficiency, a leader evaluating workflow tools, or someone curious about modern care practices, exploring soap notes offers valuable insight. In a landscape where careful, accurate communication shapes outcomes, soap notes are quietly leading the way—without losing sight of what matters most: people.
Zorotv Exposes a Conspiracy That D283ats the Industry You Depend On
YTS MX Could Shock You—No Talk About Any Normal Ending
Workjam Infected Every Minute—Here’s the Brutal Truth No One Talks About